Five Steps To Prevent The Next Pandemic
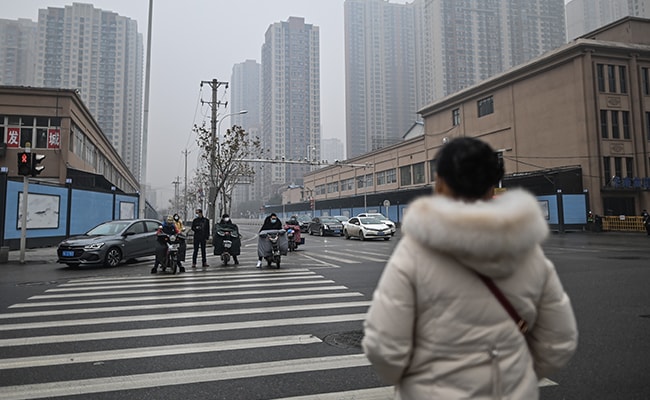
Coronavirus: More than 10 crore people across the world have contracted the virus so far.
In January 2017, a lengthy proposal showed up at the offices of the Biomedical Advanced Research and Development Authority in Washington. Running 112 pages, the document described a strategy for stopping future pandemics. It outlined a number of vaccine technologies to pursue, including messenger RNA and adenovirus vectors, and recommended that a team of 180 scientists, doctors, and other experts be created to carry out the plan. There were intricate technical details, an org chart, and an estimated cost: $595 million over 10 years.
Congress created Barda, a division of the U.S. Department of Health and Human Services, in 2006 for precisely this kind of thing. It’s charged with developing and procuring drugs and vaccines, and ensuring that the country is researching countermeasures to combat bioterrorism and chemical warfare, as well as pandemic influenza and other emerging infectious threats. The agency has historically been small, though, and the proposal, which came from the pharmaceutical company GlaxoSmithKline Plc, would have entailed one of its more ambitious efforts. Following the massive 2014 Ebola outbreak in West Africa, which killed more than 11,000 people, Glaxo researchers wanted to identify viruses likely to cause major epidemics and tackle several of them at once. “The idea was to just make vaccines against all the viruses,” says Moncef Slaoui, who was then chairman of the company’s vaccines unit and later served as chief science adviser to the Trump administration’s Operation Warp Speed.
Glaxo owned an underutilized lab and a decommissioned biotech plant in Rockville, Md., and it was already relocating vaccine researchers there as part of a corporate reorganization. Under its Barda proposal, the company would have provided scientific staff and facilities at the Rockville site while government agencies and nonprofits funded vaccine development for multiple “platform” technologies through early human trials and manufacturing. That way, if an outbreak happened, Glaxo would have prototype vaccines ready for final-stage trials.
A team from the company spent months refining the proposal, according to a person familiar with the effort, and had reason to believe it might get funded. Barda officials met with Glaxo scientists on multiple occasions, toured the Rockville facility, and urged the company to submit a formal proposal, the person recalls. After it was submitted, Barda quietly considered it for several months. Finally, in late 2017, the agency suggested that Glaxo come up with a scaled-down plan focused mainly on influenza. That proposal never got funded either, leaving the world without a key weapon against emerging viruses when the pathogen that causes Covid-19 was discovered.
Vaccines have since been developed using mRNA and adenovirus vector approaches similar to those originally suggested by Glaxo. Many of the vaccines benefited from grants from Barda during the pandemic and from government-sponsored basic research beforehand. Still, the failure to put more extensive infrastructure in place ahead of time was a lost opportunity to build up capacity that could be bolstering its vaccine supply right now. It was a failure, even a refusal, to fully plan ahead-a blunder that ranks with the White House decision to disband the dedicated pandemic response unit at the National Security Council in May 2018 and the inability of the Centers for Disease Control and Prevention to quickly develop a Covid test for wide distribution.
In late 2019 every infectious disease expert knew something like the novel coronavirus was coming sooner or later, just as they know today that Covid won’t be the last pandemic. As depressing as the current situation is, though, the next one-and there will be a next one-doesn’t have to be this bad. Shortly before his inauguration, President Biden proposed spending $20 billion to speed up vaccination rollouts. That’s a start. But a complete plan-one that can protect the U.S. from mass death, catastrophic economic damage, and (let’s hope) incompetent political leaders who squander the public’s trust-will have to be more comprehensive. It will likely involve at least five separate areas of research and investment. Most of all, it will require careful preparation.
1. Pathogen surveillance
The world can’t eliminate emerging diseases. Too many people live near animals, and there’s too much international air travel. In the 21st century alone, humanity has contended with outbreaks of SARS in 2003, H1N1 in 2009, MERS in 2012, Ebola in 2014, and now Covid. Candidates to sicken the world in the future include highly virulent filoviruses, which include the Ebola and Marburg viruses; rapidly spreading mosquito-borne flaviviruses, such as those that cause Zika and dengue fever; and bat-borne paramyxoviruses, like Nipah and Hendra.

All of these are scary. Marburg and Ebola can lead to severe vomiting, diarrhea, and bleeding; Hendra and Nipah, to deadly brain swelling. More worrisome still, we tend to wait for outbreaks to kill a few dozen people before we do anything about them. “Our current strategy is we really do let them happen,” says Peter Daszak, a veteran virus hunter at EcoHealth Alliance in New York, a nonprofit research group. Daszak suggests we approach emerging viruses the way we approach terrorist networks: Track them so we can intervene before they can wreak havoc.
Daszak, who’s spent years looking for bat coronaviruses in China and elsewhere, estimates there are about 1.7 million unknown mammal viruses, many of which could spill over into humans with just a few mutations. He and his collaborators calculate that it would cost a little more than $1 billion to identify two-thirds of these pathogens by sampling wild animal populations around the world. Doing this would give scientists clues about which viruses pose the greatest risk to humans, allowing communities situated in potential hot spots to focus on reducing spillover risk and helping governments and research institutions allocate resources for further study.
If we had a better handle on what was happening pathogenically, we could work to identify the outbreaks that have the most potential to become severe, says Caitlin Rivers, an epidemiologist at the Johns Hopkins Center for Health Security. Imagine a kind of National Weather Service for pandemics that would predict the course of emerging pathogens. These official forecasts would be more authoritative than the hodgepodge of competing disease models out there now, making it easier for governments to undertake potentially unpopular mitigation measures such as closing borders or ordering lockdowns before an outbreak takes hold.
During the Covid pandemic, the opposite happened. In late February, right before its hospitals were overrun, Milan’s city government unveiled a campaign called “Milan does not stop,” which encouraged people to visit tourist attractions and go out to dinner. In the U.S. many local leaders hesitated before imposing harsh social distancing measures. Had restrictions come only one week earlier, according to research from Columbia, 32,000 lives would have been saved by early May. “It’s about giving decision-makers enough confidence so they feel comfortable acting,” Rivers says. And an epidemic forecasting center would be a relative bargain, costing the U.S. only $100 million to $150 million a year, she estimates. The Biden administration is planning to create one.
2. Repairing and augmenting the WHO
Pandemic surveillance and response, almost by definition, are global efforts, which means it’s time to consider a new global partnership to oversee them. The World Health Organization’s structural shortcomings have been well documented. The main international body charged with fighting disease, it’s been criticized by the U.S. and others for being overly deferential to China and for being slow to declare the outbreak a global emergency. The agency responds that it has to remain diplomatic while collecting information and that it can’t force member states to reply to it. Still, the spat led the U.S. to announce last year that it was withdrawing, further weakening the body at a key moment.

This dispute, like so many aspects of the Covid catastrophe, was predictable. The current pandemic response system relies on transparency. Governments are supposed to alert the international community at the first sign of danger. But of course leaders, worried about damaging their national economies or their personal political prospects, often clam up at the crucial moment and withhold data the rest of the world needs. China was slow to admit the magnitude of the problem in Wuhan early last year and didn’t immediately let international health experts into the city to assess the threat. In the U.S., President Trump confronted the looming crisis by dismissing it, repeatedly assuring Americans that Covid would simply go away. “One day, it’s like a miracle, it will disappear,” he said on Feb. 27, just as the virus was taking off.
Thomas Bollyky, who heads the global health program at the Council on Foreign Relations, points out that none of this is new. “This is a repeated problem,” he says. China was slow to acknowledge the SARS outbreak in 2003, and in 2014 officials in West Africa took months to recognize that mysterious illnesses in remote areas were being caused by the Ebola virus, allowing it to travel from rural areas, where it probably could have been contained, to cities. In a recent report, Bollyky and his colleagues recommended developing a system that bypasses central government bureaucrats and monitors anonymized data, such as rising cases of unexplained pneumonia, gathered directly from hospitals around the world. It was a locally run project, the Seattle Flu Study, that first spotted community spread of Covid in the U.S.
In January an independent panel convened by the WHO blasted the current epidemic alert system as “slow, cumbersome, and indecisive.” In theory the WHO, which Biden has said the U.S. will rejoin, could be given more teeth. But some argue that the world might need a new coalition of countries to more effectively coordinate response. Richard Hatchett, chief executive officer for the Coalition for Epidemic Preparedness Innovations (CEPI), an organization that’s worked to accelerate the development of Covid vaccines since it started up in 2017, has suggested an alliance committed to a less cautious approach-a “biological NATO” to defend the world against developing pathogens. This group could help countries respond much more rapidly to future threats. “It’s not part of the world against any other part of the world, but the world against the viruses,” Hatchett says.
A muscular global health coalition could further provide funding to eliminate “wet markets,” where wild animals are sold for food, and to discourage jungle deforestation, which pushes animals (and the viruses they carry) into closer proximity with people. And it could help train more field workers in far-flung places instead of relying on the current ad hoc system, in which a mix of nonprofits, universities, and volunteers, along with the WHO, addresses emerging threats. “Infectious diseases are like wildfires. You need to stomp them out when they are containable,” says Anne Rimoin, an epidemiologist at UCLA. “In both cases, time is of the essence.”

Rimoin has worked on Ebola for years in the Democratic Republic of Congo. There, the megacity of Kinshasa abuts the world’s second-largest rainforest, which teems with virus-laden animals. She’s been trying to build up an infrastructure to respond to outbreaks, relying mostly on individual private donors. Sometimes she scrounges for basic gear herself, tracking down donated lab equipment in the U.S. then checking dozens of extra bags on her flights to Africa.
3. Genetic sequencing
Tracking and tracing a virus has typically been thought of as a labor-intensive process that involves building lists of patient contacts and then calling those people one at a time to see who else might have become infected. Gene sequencing, by contrast, offers the tantalizing possibility of tracking a virus’s spread with molecular precision. Frequent, intensive viral sequencing would help answer questions such as how widely a given strain spreads within a community like a school and whether the strain might mutate to become resistant to existing vaccines.
Thanks to the ubiquity of high-speed gene-sequencing machines, it costs only $50 or so to sequence a virus’s whole genome. This information provides clues for contact tracers about the pathogen’s path and allows the large-scale tracking of mutations. Unfortunately, in the U.S. only about 3 in 1,000 Covid patients have had their virus samples sequenced. And much of the work has been done in academic labs, which are removed from the front-line facilities that have access to detailed patient data and do the day-to-day contact tracing.
One of the current leaders in virus sequencing is the U.K.; it’s processed more than 200,000 samples, about 5% of its caseload. That helped Britain catch the B.1.1.7 variant, which epidemiologists say could be more transmissible. Because it was found in dozens of countries, it’s expected to become the dominant strain in the U.S. The lack of virus sequencing in the country “is a huge failing of our public-health system,” says Marc Lipsitch, an epidemiologist at Harvard. “Hopefully, this will be a wake-up call.”
Biden has recognized the problem, announcing plans to drastically build up sequencing capacity and choosing as his science advisor Eric Lander, a renowned genomics expert with the Broad Institute of MIT and Harvard.
4. Developing more vaccines, faster
Vaccines have been the most spectacular success story so far in the current pandemic. There are already two highly effective options on the U.S. market, and a third vaccine from Johnson & Johnson could be cleared within weeks, after the company reported Phase III results on Jan. 29 showing that it generated strong protection against severe Covid. Yet there’s clear opportunity for improvement. “We need to have strategies that allow us to move even faster,” says David Ho, who leads the Aaron Diamond AIDS Research Center at Columbia. Ho estimates we could have easily shaved four to five months from the drug and vaccine timeline had more preparation taken place.

Early investment in mRNA technology by the U.S. government helped Moderna Inc. bring its vaccine candidate to human trials in a record 66 days. But it still required more than four months of Phase I and Phase II trials to confirm safety and find the right dose before the crucial Phase III trial could begin in late July. There’s no available shortcut around this final stage, which focuses on efficacy in humans, but Moderna could have tested candidates for known coronaviruses ahead of time, which might have allowed it to start a large Phase III trial months earlier, according to CEO Stéphane Bancel. “Fall would have looked so different if we had a vaccine in July,” he says.
Bancel figures it would cost $200 million to $300 million to bring prototype mRNA vaccines for the 10 most worrisome virus classes through early human trials, so that with a few tweaks, they’d be ready for large-scale testing. It might cost another $1 billion or $2 billion to maintain a spare manufacturing plant along with a stockpile of raw materials for millions of doses. In January, in a small start toward this goal, Moderna announced that it’s begun work on a vaccine for the Nipah virus, which has killed hundreds in multiple outbreaks in Asia since 1999.
Bancel’s proposal is similar to the concept Glaxo tried to sell Barda on back in 2017. A spokeswoman for the Department of Health and Human Services says that at the time, Barda’s funding from Congress was focused on defending against influenza and biological, chemical, and radiological weapons; it’s now soliciting proposals for coronavirus countermeasures, including vaccines. Some people also saw the proposal as too tightly linked to one company and in competition with groups such as CEPI, which has backing from the Bill & Melinda Gates Foundation and others to develop vaccines against emerging threats. Glaxo declined to go into detail on why it couldn’t attract funding, but in a statement it said it’s committed to pandemic-related research efforts.
One tantalizing area for future investment: vaccines and drugs that offer protection against multiple viruses. The existing Covid vaccines spur antibodies against the unique spike protein the virus uses to enter cells. Researchers could instead create a shot that triggers an immune response against the stem of these spikes, which varies much less between strains, allowing protection against numerous Covid-like illnesses at once, according to Vineet Menachery, a coronavirus specialist at the University of Texas Medical Branch at Galveston. It’s tricky and it might not work, but the potential payoff would be immense. In November the National Institutes of Health announced plans to fund research into broad-acting coronavirus vaccines.
Something similar should be done with antiviral drugs, says Ralph Baric, a coronavirus researcher at the University of North Carolina who did crucial research before the pandemic showing that remdesivir, an antiviral developed by Gilead Sciences Inc. to fight Ebola, was promising against coronaviruses. Remdesivir got cleared for the U.S. market on May 1 in part because it had already been tested extensively in patients during a 2018 outbreak in the DRC, so only Phase III trials targeting Covid were required. But remdesivir must be administered through an IV, which has limited its use to hospitalized patients. Merck & Co. is working on a coronavirus drug that could be taken as a pill, but unlike Gilead’s medicine, it hadn’t yet started Phase I trials at the start of the pandemic, putting it on a much slower path. Efficacy trial results are expected by April.
5. Ironing out distribution and logistics
Getting tests and vaccines to people isn’t rocket science. It’s not even regular science. But adapting logistics in a medical system as large and complicated as that of the U.S. can take months of advance planning and coordination, and databases must be developed to keep track of everything. Not enough of that work happened in 2020, as the Trump administration insisted on having state governments handle testing, acquire and distribute personal protective equipment, and implement vaccine distribution protocols.
This has arguably been, in retrospect, the most unfortunate and most easily avoided failure. “A national and international crisis needs the full intervention of the federal government,” says Peter Hotez, a vaccine researcher and dean of the National School of Tropical Medicine at Baylor College of Medicine in Houston. “It’s one of the major reasons we’ve lost 400,000 American lives, because of this bizarre insistence.”

Biden’s plan to have the federal government set up mobile clinics and community vaccination centers in gymnasiums and stadiums could spur things along. (It probably should have been the plan from the beginning.) But once we’re through the immediate crisis, the U.S. needs to take stock of its supply chains for basic drugs, equipment, and testing supplies-and then to provide incentives for companies to create more capacity where it’s needed. “Our federal government has no idea what supply chains are vulnerable,” says Julie Swann, a health-systems expert at North Carolina State University. When Hurricane Maria slammed into Puerto Rico in 2017, it shut down power to one of the biggest U.S. makers of saline IV bags, exacerbating an existing shortage of an essential medical item. This year, to name one of many examples, a shortage of plastic pipette tips needed for automated laboratory machines slowed down Covid testing, forcing labs into a constant scramble for supplies.
Not only do we have no effective way to count basic medical staples, but we’re also unable to keep proper track of public-health data on patients and testing capacity; it’s all logged in a hodgepodge of outdated and often incompatible federal, state, and local computer systems. Not knowing where outbreaks are worst makes it difficult to identify where to send supplies. “We’re flying blind,” Swann says. State databases need “more integration so we know in real time where our inventory is.”
During the current crisis, all of this has been harder than it needed to be. That’s because pandemic response requires foresight, something that was in short supply the past few years. “Nobody ever expected a thing like this,” Trump said on March 24, in one of his many false statements about the virus. Many experts had, in fact, been predicting a pandemic for years, but they couldn’t persuade anyone to do enough about it.
Slaoui, the former Operation Warp Speed adviser, says policymakers seem to care about fighting epidemics only shortly after they’ve happened. “When the outbreak is there, every government is all over you as an industry,” he says. “And then when the outbreak dissolves, everybody looks the other way.”
That’s what happened in too much of the world after SARS, MERS, and Ebola. With 2 million dead worldwide and a year’s worth of economic devastation, it should be harder to look the other way now.
(Except for the headline, this story has not been edited by NDTV staff and is published from a syndicated feed.)